Heart Valve Voice Canada and Shoppers Drug Mart Join Forces to Raise Awareness of Heart Valve Disease
Heart Valve Voice Canada, the country’s leading patient advocacy organization for heart valve disease (HVD), today announced a national partnership with Shoppers Drug Mart to improve the early detection and management of HVD across Canada.
Earlier treatment for asymptomatic severe aortic stenosis may save lives
Recent research shows that early treatment reduced death and hospital visits for heart failure in certain people with aortic stenosis.
Digital stethoscopes and AI may improve valve disease detection
A study led by Canadian researchers will determine if digital stethoscopes and AI can more accurately detect heart murmurs than traditional stethoscopes.
Listening Saves Lives: Supporting Early Detection for Heart Valve Disease
Heart Valve Voice Canada raises awareness through free stethoscope checks in communities across Canada—early detection of heart valve disease can save lives.
It’s Official: Ontario is First to Proclaim Heart Valve Disease Awareness Act
Heart Valve Voice Canada is celebrating the passing of Bill 66, the Heart Valve Disease Awareness Act, a Private Members’ Bill sponsored by MPP Rudy Cuzzetto, in the Ontario Legislature.
Global Heart Hub’s Unite Summit 2024: A Global Gathering for Heart Patient Advocacy
Heart Valve Voice Canada’s Managing Director, Ellen Ross shares summit highlights including the transformative power of patient advocacy in driving meaningful change.
The New England Journal of Medicine featured this research study in October 2024
The study found that patients with severe asymptomatic aortic stenosis fared better with early intervention by minimally invasive surgery than with clinical monitoring every six to 12 months. Monitoring is the current practice.
The research study was co-authored by Dr. Philippe Pibarot, a Heart Valve Voice Canada board member.
Cardiovascular Disease Conference opens with powerful patient story by Heart Valve Voice Canada board member
Len Crispino shared his patient story about living with multiple heart conditions, kidney failure and cancer in a video to open the November 2024 Unite Summit.
Screening program raises awareness of valve disease
Heart valve disease is common and treatable, yet too few people know they could be at risk. Now, mobile clinics from the University of Ottawa Heart Institute are screening people in the Ottawa area for valve disease and other heart conditions. The clinics target individuals 65 years or older focusing on underserved communities, including rural residents and Indigenous people, and aim to get patients to the care they need faster.
Growing awareness, better support
More people are becoming aware of heart valve disease, and more people living with valve conditions are getting support and information to manage their health. These are just some of the ways Heart Valve Voice Canada — the country’s only national, patient-led heart valve organization — is making a difference. Learn more in our 2023 Impact Report.
Achieving early detection and diagnosis for cardiovascular disease: A manifesto for change
The first patient-led global manifesto calling for early detection and diagnosis of cardiovascular disease is available now, and Heart Valve Voice Canada was delighted to contribute!
Heart Valve Disease: Working together to create a better patient journey
The report Heart Valve Disease: Working together to create a better patient journey commissioned by Heart Valve Voice Canada and written by The Health Policy Partnership provides a comprehensive view of the entire heart valve disease patient journey from first detection to diagnosis, follow-up, and treatment, identifying gaps and their impacts. This report was developed under the guidance of a multidisciplinary advisory council, whose members included people with lived experience and healthcare professionals engaged in heart valve disease in Canada. The patient perspective was the common thread throughout this report.
Paving the way: a roadmap to the successful implementation of shared decision-making in heart valve disease
This global roadmap, to which Heart Valve Voice Canada is a contributor, is designed to support patient organizations and advocates who wish to implement shared decision-making for people facing heart valve disease treatment options.
Hugh MacPhie announced as Heart Valve Voice Canada Chair
We are pleased to announce Hugh MacPhie as the new Heart Valve Voice Canada Chair. Having joined the board in 2022 Hugh will build on the board’s mission to grow it's reach and impact.
Heart Valve Voice Canada forms new partnership to help raise awareness amongst seniors
In an exciting new partnership, the Canadian Cardiovascular Society, Heart Valve Voice Canada, and MediSystem Pharmacy are teaming up to put a spotlight on heart valve disease and improve early detection for those most at risk.
HVVC welcomes three new distinguished Board Members
As we work towards our mission to improve the health and quality of life for people living with heart disease, a key part of our action plan involves finding the right partners to drive our patient advocacy forward. Our Heart Valve Voice Canada Board of Directors is the heartbeat of our organization and we are continually looking for advocates who will help us empower people and save lives. We are honoured whenever someone volunteers their skillset and time to our mission, and we are happy to announce a few new additions to our team.
Be prepared for your upcoming hospital stay
Packing the right items and being prepared for your hospital stay can remove some of the stress of your upcoming treatment. Anticipating what you will need when you come home can also help you focus on your recovery and support your journey back to an active life.
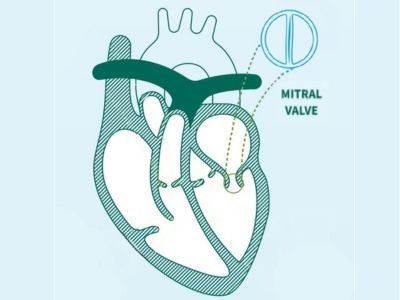
Better access to care for mitral valve patients in Saskatchewan thanks to champion efforts by local cardiologist
Heart valve disease patients who live in Saskatchewan and are candidates for a transcatheter mitral valve repair procedure, can now get the procedure done in their home province, avoiding personal out-of-province travel costs, health risks, and accompanying stress.
Solving for heart valve disease is solving for healthy and active aging
Early screening of heart valve disease saves public health care systems resources, but prevalent ageism delays diagnosis, limits care, and leads to avoidable costs and impacts on people’s lives.
Heart Valve Disease Awareness Act passes first reading
All MPPs and staff at Queen’s Park in Toronto were invited to participate in the #ListenToYourHeart Challenge reception. MPP Rudy Cuzzetto introduced Bill 66, The Heart Valve Disease Awareness Act, proclaiming February 22nd as Heart Valve Disease Awareness Day in Ontario. During the reception, the landmark report, Heart Valve Disease: Working together to improve the patient journey was shared with key decision makers. More than 90 policy makers and staff participated and showed their support.